|
Chronic pain can make it easy to feel overwhelmed, reduce our activity levels, and become isolated. Goals help restore a sense of order, build self-efficacy and sense of control, improve mood, and provide direction by helping with planning daily activities.
One of the tools we learned at the Mayo Clinic Pain Rehabilitation Center was goal setting to help us plan our days and keep us on track. We set goals each day. They didn't have to be massive, but they had to be SMART - specific, measurable, achievable, relevant, and time-bound.
Some SMART goal examples:
Did you notice none of the goal examples included pain reduction? Our focus should be on reducing stress, improving our quality of life and increasing functional ability and activity, not pain reduction. Focusing on pain reduction is an easy trap to fall into - leading to frustration and depression. Just as the homepage of my website says - we can live well, despite the pain. Celebrate! While it's natural to celebrate big goals, be sure to celebrate milestones along the way, as well as smaller victories. These celebrations keep us motivated along the way and help instill confidence. Resource Pain is the body’s alarm system. It’s designed to protect us from danger just like a home security system or a smoke detector. It’s the body’s normal response to acute tissue damage or injury and heals in normally 3-6 months.
But what happens when pain doesn’t go away? Once pain persists beyond the normal healing time, it becomes chronic - losing its warning function and becomes its own disease/condition. It’s an abnormal response (with or without obvious pathology). Although all pain hurts, not all pain indicates damage. We know what to expect from our pain by the very nature of it being chronic or ongoing. It’s not like getting burnt, twisting an ankle, or getting stung by a bee that needs protection until the injury has heals. Of course, any unexpected new pain should be investigated. Learn more
Pain, stress, and tension are closely related. Muscles tighten and put pressure on nerves resulting in even more pain.
It’s possible to activate your body’s natural relaxation response to help reduce the tension using mind-body tools like:
Helpful videos
Free Apps FIND MORE TOOLS AND APPS Updated 3/1/24
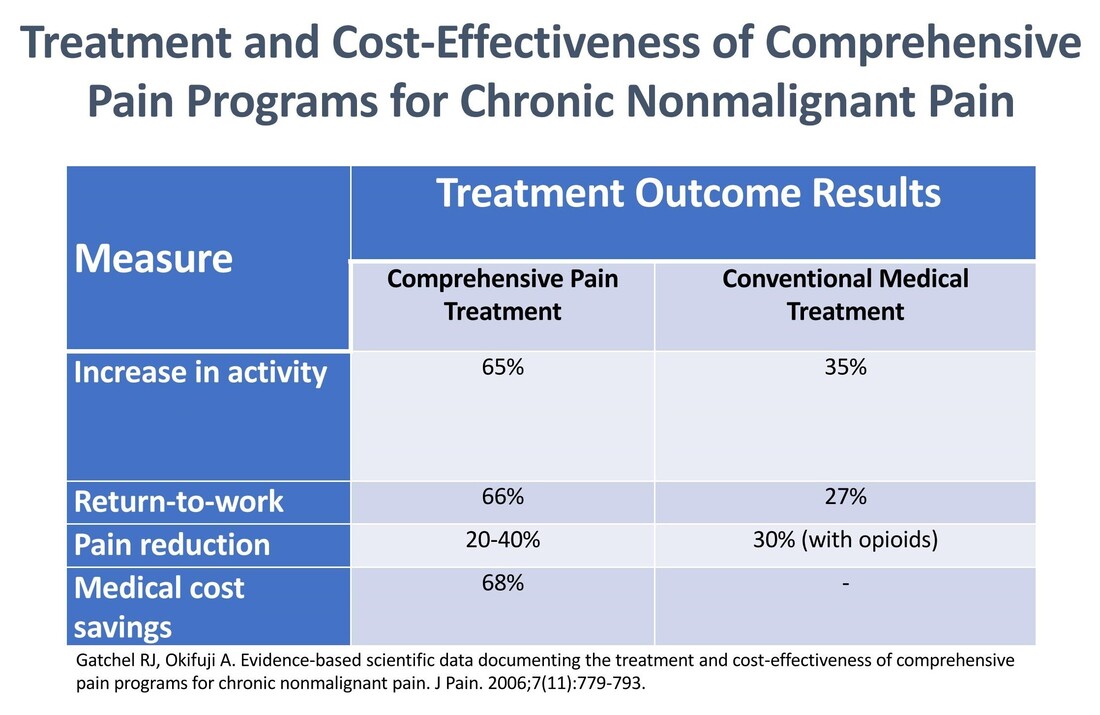
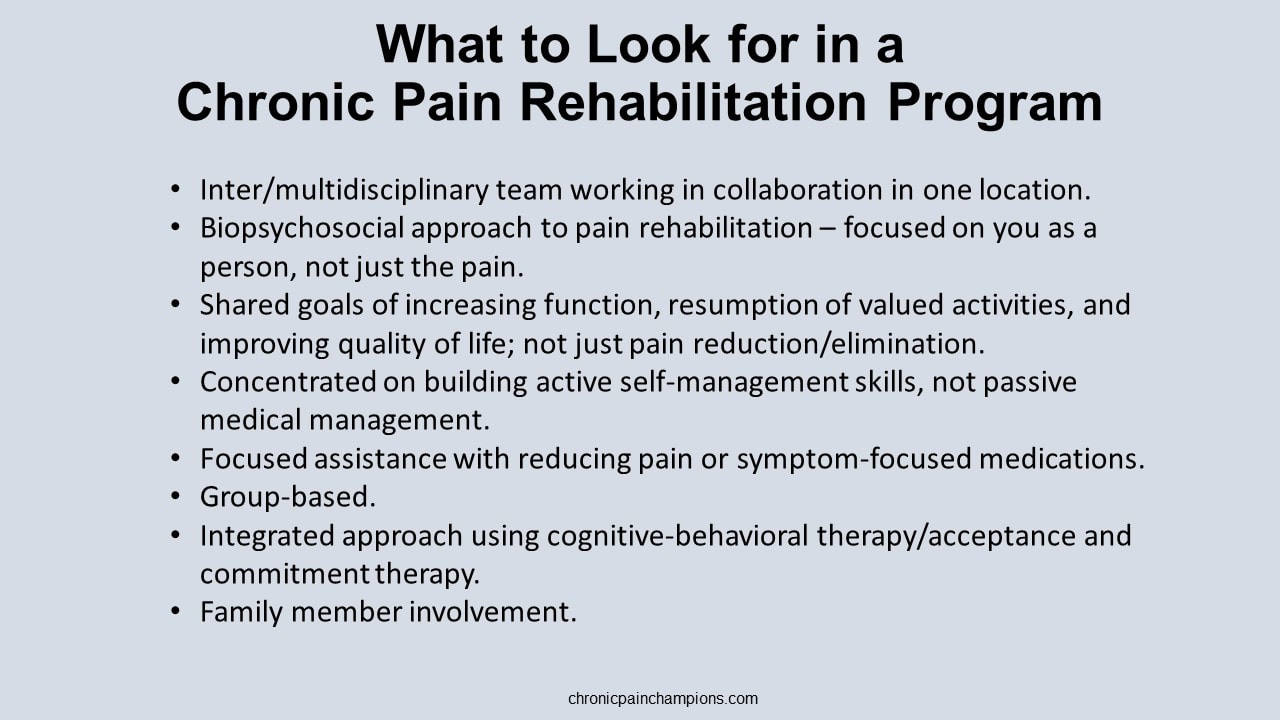
Pain rehabilitation goes beyond medicine and medical interventions – and crosses different disciplines. It doesn’t just focus on removing the pain. It focuses on the patient and how they can play a role in their own pain management - giving them control over the pain instead of letting the pain control them.. It’s a proven approach based on the biopsychosocial model of medicine – benefiting patients while reducing costs and reliance on the medical system. In addition to their general efficacy, these types of programs using interdisciplinary chronic pain rehabilitation can be effective at weaning patients off opioid therapy with long-term improvements in pain, mood, and function. I was fortunate to be able to attend the 3-week interdisciplinary Mayo Clinic Pain Rehabilitation Center – not just once, but twice. It was both a game-changer and lifesaver for me. I highly recommend the program to anyone interested in taking an active role in managing their own care. Read about my Mayo experience in this article. More programs like this are needed to shift the current reliance on biomedical therapy towards a greater reliance on provider-supported patient self-management and true biopsychosocial treatment. . Availability is important but so is accessibility. These programs aren't cheap, and insurance can be hesitant the pay the price tag. What payors need to remember is that these programs are cost-effective with a 68% reduction in medical cost spending. Find links to programs in the U.S. and around the globe. What to look for in a program A pain rehabilitation program should focus on you as a person, not just your pain. Interdisciplinary pain rehabilitation programs that take place in the same facility with health care providers working together with open communication and shared objectives are the gold standard of comprehensive care outperforming medical pain services and less coordinated multidisciplinary programs. A comprehensive pain rehabilitation program typically includes:
Learn more about pain rehabilitation
Pro golfers use visualization when they play. They picture the precise shot they want to hit before taking the club back – the trajectory, shape, roll and finish. This puts a positive image in the mind; the body then makes the motions needed to turn the image into reality.
We can do the same with our pain. We can visualize a different way to view our pain and respond to it. We can visualize living well despite the pain. And we can visualize the pain leaving our bodies or the pain taking a smaller role in our lives. Try these exercises
Find links to these and other self-management tools. I was recently honored to be a guest on the Compass Opioid Stewardship Program podcast hosted by Dr. Rachael Duncan, PharmD. and Dr. Don Stader.
I'm so grateful for the opportunity and blessed to be able to share my story with clinicians. I'm also thankful for the generosity of Dr. Stader. You'll find out what he offered me at the end of the podcast. It brought me to tears. You can listen to the podcast episode on Apple, Spotify, and Libsyn via the links below: Check out the entire podcast series. Learn more about the Compass Opioid Stewardship Program. |
Categories
All
Archives
July 2024
CHRONIC PAIN CHAMPIONS, LLC AND THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
All information is for educational purposes only. Use at your own risk. By accessing/using this website and any related pages/information/products/services, you agree to the terms and conditions. PLEASE SEE THE DISCLAIMER PAGE TO LEARN MORE. ©2024 Chronic Pain Champions, LLC All rights reserved. For personal, non-commercial use. |