|
(updated 12/12/23)
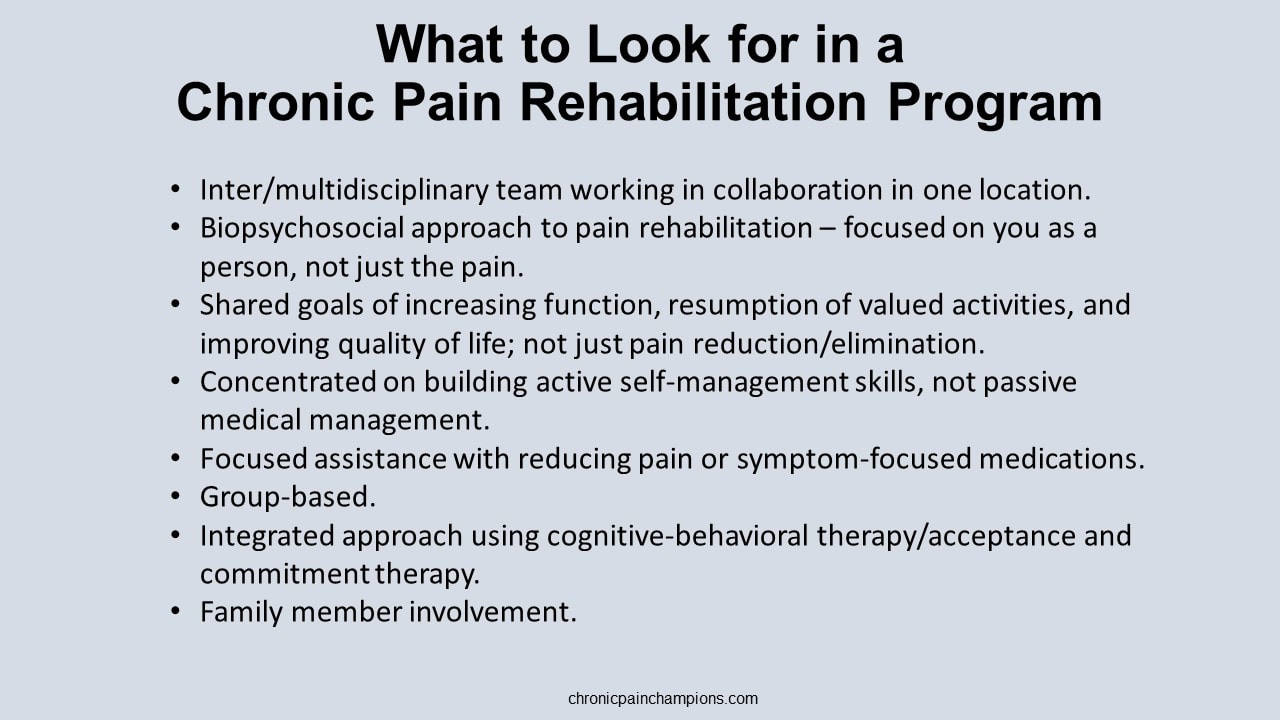
Has your doctor referred you to pain management but you’re unsure where to go and what to expect? With all the different names such as pain clinics, pain centers, pain management centers, pain treatment centers, pain institutes, pain management programs, and pain rehabilitation programs, it’s easy to get confused. I’ve tried to separate the different types of treatment facilities below into broad categories based on their disciplinary approach and treatment focus with a chronic pain rehabilitation rating. GOOD Intradisciplinary interventional pain management: Pain management physicians (typically anesthesiologists) provide an individualized approach to evaluate, diagnose, and treat all different types of pain frequently focusing on the cause of pain, pain reduction or elimination, and specific pain conditions. They primarily offer passive interventional procedures such as medications, injections, spinal procedures, nerve blocks, radiofrequency ablation, Ketamine IV therapy, acupuncture, pain pumps, spinal cord stimulators, and surgery. Multidisciplinary pain management: Pain management specialists provide interventional treatment with access or referral to other specialties like physical therapy, psychology, neurology, surgery, orthopedics, acupuncture, nutrition, and pharmacy with treatment customized to each patient based on their condition. While these providers may work in the same facility or for the same employer, they often operate independently with their own modalities and therapeutic goals. BETTER Multidisciplinary pain rehabilitation: A core provider team from multiple disciplines (physical therapy, psychology, rehabilitation medicine, anesthesiology, nursing, and occupational therapy) with additional involvement from surgeons, neurologists, internists, physiatrists, psychiatrists, social workers, dietitians, and pharmacists use the biopsychosocial model of medicine and standardized treatment approaches to help manage pain. Featuring psychological and behavioral therapies, traditional medicine, physical reconditioning, and educational components, these multi-week programs are more comprehensive but can be combined with interventional pain therapies for specific pain conditions. Care may or may not be coordinated or integrated with shared goals. BEST Interdisciplinary pain rehabilitation: Features a diverse multidisciplinary team including physical and occupational therapists, psychologists, dieticians, pharmacists, nurses, and medical doctors at one location. The providers interact with each other and the person using a shared biopsychosocial approach to pain – working together toward a common and coherent goal of pain rehabilitation teaching skills to empower the person to help themselves and actively self-manage the pain with the goals of reducing fear of exercise and activity, increasing daily activity; improving physical reconditioning; decreasing healthcare utilization, and improving quality of life with some but less focus on reducing pain. Generally lasting several weeks, these programs are often hospital-based (6-8 hours per day) and group-based offering behavioral therapy, physical therapy, occupational therapy, relaxation training, medication optimization/management, as well as some sort of family education and counseling. Conclusions/thoughts
It was my family doctor and a local surgeon who recommended I attend the 3-week outpatient Mayo Clinic Pain Rehabilitation Center instead of going through another risky surgery to try to fix the pain. The program changed my life. Please discuss your medical situation with your healthcare team. Learn more
I was blessed to see Nik Wallenda (the famous tightrope walker who has walked across the Grand Canyon, Niagara Falls, and Times Square) perform while I was on vacation.
As impressive as Nik's balancing skill was the message he shared about not giving up and overcoming fear. He almost gave up tightrope walking after a 25-foot fall during a 2017 rehearsal for an eight-person pyramid routine seriously injured five of his friends and family members. Luckily, Nik and two others were able to catch the rope and avoid falling. Like Nik, it’s important for us to overcome any fears we may have about pain and keep moving forward. You can see the accident and learn more here. Related resources
"Pain is physical AND emotional 100% of the time."
- Dr. Rachel Zoffness Pain is an experience with biopsychosocial factors, including our emotions. Often times, people living with chronic pain can become angry and less thankful. There may even be some perceived misjustice, as was in my case. It can be helpful to let go of the unpleasant emotions like anger, unappreciation, and blame as they can negatively affect the chronic pain experience, disrupt relationships, and worsen our symptoms – turning up the pain volume. While being forgiving, kind, and grateful won’t magically make the pain disappear; they can help lessen the pain and suffering, foster better health, build self-efficacy, and make life more enjoyable. Learn more and learn how
Read the research
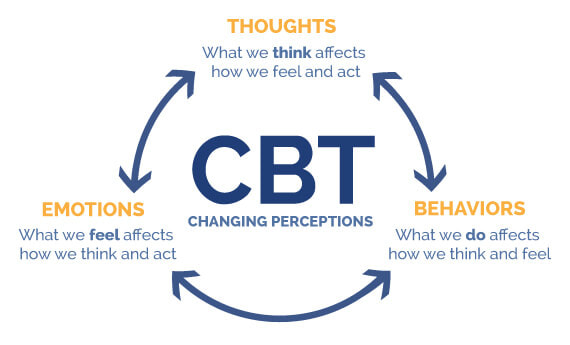
Updated 09/23/2023 Our thoughts, emotions, and behaviors can make pain worse or more manageable. We can change the pain experience and retrain our overprotective pain systems by changing how we think, feel, and behave using a form of biopsychosocial treatment called Cognitive Behavioral Therapy (CBT). CBT reprograms our minds and bodies to help us feel safe and confident in our ability to manage pain and do the things we enjoy — improving the body’s natural pain relief mechanisms, increasing function, and breaking the chronic pain cycle. .CBT is based on the core principles that our thoughts, emotions, and behaviors interact together with the pain; that we can become trapped in unhelpful thoughts, emotions, and behaviors; and that we can modify our thoughts, emotions, and behaviors to make our experience more manageable. It's what changed my pain experience and my life by giving me tools to:
Best yet, CBT is a do -it-yourself therapy. You can use it anytime. You don’t need help from anyone once you learn it. And there are no negative side effects. I learned CBT while attending the prestigious 3-week interdisciplinary Mayo Clinic Pain Rehabilitation Center. Find a CBT pain therapist It can be hard to find psychologists trained in cognitive behavioral therapy for pain. Ask them about their approach to treatment. You might want to use the content from my pain truths and pain quiz to see if they match the latest pain science. Theres are links to therapist search tools and pain rehabilitation programs below. Learn more and do more
Image courtesy of McGovern Medical School
|
Categories
All
Archives
July 2024
CHRONIC PAIN CHAMPIONS, LLC AND THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
All information is for educational purposes only. Use at your own risk. By accessing/using this website and any related pages/information/products/services, you agree to the terms and conditions. PLEASE SEE THE DISCLAIMER PAGE TO LEARN MORE. ©2024 Chronic Pain Champions, LLC All rights reserved. For personal, non-commercial use. |