|
"In a word, describe how you feel right now."
I recently saw this question asked in a 99,000-member fibromyalgia support group. Almost all the 377 answers just two days after the post had negative connotations. Words like exhausted, defeated, overwhelmed, afraid, lousy, anxious, depressed, painful, lifeless, restricted, broken, irritable, lost, done, and disconnected were shared. The few positive answers included words like confident, grateful, proud, and hopeful. The overwhelming percentage of negative words saddens me about the level of pain care and what people living with pain are experiencing. My answer was confident. However, there was a time in my journey with chronic pain when my answer wouldn't have been as positive. That was before I attended a pain rehabilitation program, accepted the pain, and learned to live well despite it using active self-management strategies. We need to stop treating chronic pain as prolonged acute pain because it's not prolonged acute pain. It is its own condition. Clinicians need to empower people living with pain – shifting from a "find-it, fix-it" mentality to a "self-management" mentality. Learn more
(updated 12/12/23)
Has your doctor referred you to pain management but you’re unsure where to go and what to expect? With all the different names such as pain clinics, pain centers, pain management centers, pain treatment centers, pain institutes, pain management programs, and pain rehabilitation programs, it’s easy to get confused. I’ve tried to separate the different types of treatment facilities below into broad categories based on their disciplinary approach and treatment focus with a chronic pain rehabilitation rating. GOOD Intradisciplinary interventional pain management: Pain management physicians (typically anesthesiologists) provide an individualized approach to evaluate, diagnose, and treat all different types of pain frequently focusing on the cause of pain, pain reduction or elimination, and specific pain conditions. They primarily offer passive interventional procedures such as medications, injections, spinal procedures, nerve blocks, radiofrequency ablation, Ketamine IV therapy, acupuncture, pain pumps, spinal cord stimulators, and surgery. Multidisciplinary pain management: Pain management specialists provide interventional treatment with access or referral to other specialties like physical therapy, psychology, neurology, surgery, orthopedics, acupuncture, nutrition, and pharmacy with treatment customized to each patient based on their condition. While these providers may work in the same facility or for the same employer, they often operate independently with their own modalities and therapeutic goals. BETTER Multidisciplinary pain rehabilitation: A core provider team from multiple disciplines (physical therapy, psychology, rehabilitation medicine, anesthesiology, nursing, and occupational therapy) with additional involvement from surgeons, neurologists, internists, physiatrists, psychiatrists, social workers, dietitians, and pharmacists use the biopsychosocial model of medicine and standardized treatment approaches to help manage pain. Featuring psychological and behavioral therapies, traditional medicine, physical reconditioning, and educational components, these multi-week programs are more comprehensive but can be combined with interventional pain therapies for specific pain conditions. Care may or may not be coordinated or integrated with shared goals. BEST Interdisciplinary pain rehabilitation: Features a diverse multidisciplinary team including physical and occupational therapists, psychologists, dieticians, pharmacists, nurses, and medical doctors at one location. The providers interact with each other and the person using a shared biopsychosocial approach to pain – working together toward a common and coherent goal of pain rehabilitation teaching skills to empower the person to help themselves and actively self-manage the pain with the goals of reducing fear of exercise and activity, increasing daily activity; improving physical reconditioning; decreasing healthcare utilization, and improving quality of life with some but less focus on reducing pain. Generally lasting several weeks, these programs are often hospital-based (6-8 hours per day) and group-based offering behavioral therapy, physical therapy, occupational therapy, relaxation training, medication optimization/management, as well as some sort of family education and counseling. Conclusions/thoughts
It was my family doctor and a local surgeon who recommended I attend the 3-week outpatient Mayo Clinic Pain Rehabilitation Center instead of going through another risky surgery to try to fix the pain. The program changed my life. Please discuss your medical situation with your healthcare team. Learn more
It’s common for patients to talk about pain levels and treatments with family and friends. Although talking about pain can help us validate our experience, it can actually worsen our symptoms by adding more attention to the pain.
You can’t make positive steps in your life when surrounded by negativity Stay away from people who only want to complain about pain, and avoid sharing the pain with others unless there is a positive goal associated with the conversation. Talk instead about things you enjoy and find meaningful. Fill your life with joy and hope! It’s natural for people to ask about the pain, but you have the power to change the discussion. Thank them for asking but explain that you’d rather focus on something else. Suggest a more life-affirming topic of conversation. I choose not to talk about the chronic pain I feel to myself or with others, including my doctors (unless there is a new symptom that needs acute treatment). Learn more
"Pain is physical AND emotional 100% of the time."
- Dr. Rachel Zoffness Pain is an experience with biopsychosocial factors, including our emotions. Often times, people living with chronic pain can become angry and less thankful. There may even be some perceived misjustice, as was in my case. It can be helpful to let go of the unpleasant emotions like anger, unappreciation, and blame as they can negatively affect the chronic pain experience, disrupt relationships, and worsen our symptoms – turning up the pain volume. While being forgiving, kind, and grateful won’t magically make the pain disappear; they can help lessen the pain and suffering, foster better health, build self-efficacy, and make life more enjoyable. Learn more and learn how
Read the research
Updated 3/27/24
Some people find medical cannabis helpful for chronic pain, especially in the short term, but there are questions about long-term effectiveness and safety. Cannabis wasn’t recommended by Mayo Clinic when I attended their Pain Rehabilitation Center in 2018 nor is it recommended by the International Association for the Study of Pain. A new systematic review and meta-analysis published November 28, 2022, in the Journal of the American Medical Association, suggests cannabis is no better at relieving pain than a placebo. And relying on any sort of passive treatment like medicines and supplements can create dependence on the agent - producing a sense of helplessness and reminding the user of the pain. I have found I don’t need medicine or supplements to manage my chronic pain. Of course, your experience may differ. I know mine did earlier in my pain journey. My relief came by changing how I think about, feel about, and behave around the pain with pain rehabilitation using self-management. Learn more
Updated 04/11/2024
Back pain can be scary, especially when an MRI finds something abnormal. While they can seem scary, structural findings on a diagnostic scan don’t always equate with pain or are the cause of the pain. Abnormal MRI findings are normal in people without pain, especially as age increases. Over 50% of 30-year-olds with no pain show signs of disk degeneration increasing up to 80% at age 50 (Brinjikji, et al, 2015). And although chronic back pain is a common medical complaint, no specific cause is found in up to 85% of cases with central sensitization as a potential contributing factor (Sanzarello, et al, 2016) along with fear of pain and activity as maintaining factors. Remember, all pain is biopsychosocial contributors Research has found that "when individuals with low back pain consider they have a flare, they do not always have greater than average pain, but have worse psychosocial features" (Costa, et al, 2021). Read the World Heath Organization's guideline for non-surgical management of chronic primary low back pain. Check out these back facts from OSullivan, et al, 2020:
Learn more
(Updated 06/10/2024)
My article published in Health Central (formerly Practical Pain Management) "We Have a Chronic Pain Problem, Not a Prescription Opioid Problem" explored the efficacy and safety of opioids for chronic pain as well as the need for more pain rehabilitation programs. Below is some of the original content I submitted that didn't make the published version of the article which helps provide some additional context. The rise of prescription opioids In the 1990s and the next two decades, opioid prescriptions became the quickest and least expensive treatment option for chronic noncancer pain. Their rise in popularity was due to a mix of factors, including:
With the increase in opioid use came an increase in opioid use disorders and opioid deaths. Then came a hard push to reduce opioid prescriptions following the 2016 Centers for Disease Control (CDC) guidelines for prescribing opioids. The 2016 CDC guidelines indirectly led to many chronic pain patients being forced to lower their medicine doses or to stop them completely. Often with little or no tapering and no alternative treatments offered or covered by insurance. Pushing patients to undergo invasive procedures like injections or surgery. And labeling patients as “addicts” for wanting pain relief. Which all led to increased tension between patients and providers, more patient suffering, illegal drug use, or, even worse, suicide. Opioid users don’t know what they don’t know – “try it, you may like it” Unfortunately, there isn’t a crystal ball when it comes to pain treatment. There's no way of knowing how a patient will respond to any specific type of therapy. And tapering can be hard. Chronic pain patients can be weary of tapering opioids for fear of increased pain and the general fear of the unknown. Patients need to accept the possibility of worse pain and other symptoms during a taper. It’s also important for providers to remember to treat the entire person in pain and not just manage the taper. Transitioning to self-management built around pain rehabilitation takes time. It’s a marathon, not a sprint, and requires work from both the provider and the patient. It’s like the old joke “How do you get to Carnegie Hall? Practice, practice, practice.” Opioid treatment is a decision between the provider and patient The use of opioids is a shared provider-patient decision based on risk and reward including the history and needs of the patient and should be applied on a case-by-case basis. If the decision is to reduce or stop opioid therapy, tapering should be done with education about the benefits of opioid reduction and provider oversight. If the decision is to use opioids, they should be prescribed at the safest lowest dose. Either decision should include pain rehabilitation and self-management strategies.
Personal note My chronic pain recovery started after I accepted the pain and stopped doctor-shopping to find pain relief and a medical cure (many praises for the Mayo Pain Rehabilitation Center). Through pain rehabilitation, I learned how to self-manage my condition. This process led me to stop the use of medicines including opioids, benzodiazepines, anticonvulsants, muscle relaxers, amphetamines, beta-blockers, antidepressants, and over-the-counter analgesics as well as other passive interventions like supplements and injections for my pain. There's still a core you despite the pain.
What you can do
Updated 7/19/24
Do you know?
Editor’s note: This article was written based on my experience and what I have researched about the topic. Everyone is different. The decision to use supplements should be a decision between the doctor and the patient. Many people use supplements are as part of their pain treatment approach, supplements come with risk, including contamination with toxins, health problems, unwanted side effects, and interactions with conventional medicines. Limited oversight Unlike prescription or over-the-counter drugs, which must be approved by the Federal Drug Agency (FDA) before they can be marketed, the FDA doesn’t review supplements for safety and effectiveness before they are sold. We don’t know where the products are made, how they are made, what is in them, and if the dosage is appropriate. Safety is left up to the manufacturers and distributors of the supplements. My experience As part of the multi-day Mayo Clinic fibromyalgia program I attended in 2016, I met with a pharmacist to review the long list of prescription medicines, over-the-counter medicines, and supplements I was taking at the time. My medicine cabinet looked like a GNC store. I was instructed to bring the actual bottles with me to the appointment, so I packed the bottles into a gym bag (yes, I was taking a lot of medicines and supplements) and went to see her. I was surprised as she read each bottle, making comments and recommendations about each pill – including product quality, labeling issues, ingredient safety, and dosing. When the appointment ended, my medicine and supplement list was much shorter with her recommending stopping most of the supplements and my gym bag much lighter – throwing away the pills was going to stop taking. I kept only one supplement - Vitamin D. Bottom line You assume all risk when using supplements. While some may be helpful, many aren’t and some may even be harmful. And remember, that each time you take a pill or supplement, you are reminding yourself you're in pain - reinforcing the neural pathways and keeping you in the pain cycle. Review any supplements with your medical team to help you make an educated decision. Learn more
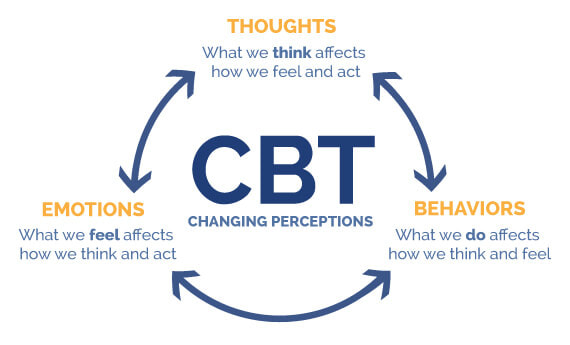
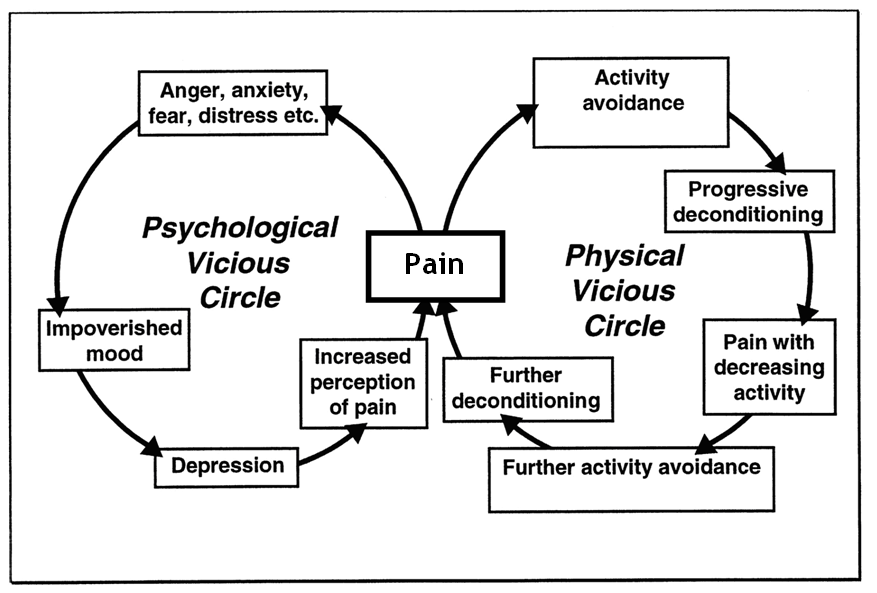
Updated 09/23/2023 Our thoughts, emotions, and behaviors can make pain worse or more manageable. We can change the pain experience and retrain our overprotective pain systems by changing how we think, feel, and behave using a form of biopsychosocial treatment called Cognitive Behavioral Therapy (CBT). CBT reprograms our minds and bodies to help us feel safe and confident in our ability to manage pain and do the things we enjoy — improving the body’s natural pain relief mechanisms, increasing function, and breaking the chronic pain cycle. .CBT is based on the core principles that our thoughts, emotions, and behaviors interact together with the pain; that we can become trapped in unhelpful thoughts, emotions, and behaviors; and that we can modify our thoughts, emotions, and behaviors to make our experience more manageable. It's what changed my pain experience and my life by giving me tools to:
Best yet, CBT is a do -it-yourself therapy. You can use it anytime. You don’t need help from anyone once you learn it. And there are no negative side effects. I learned CBT while attending the prestigious 3-week interdisciplinary Mayo Clinic Pain Rehabilitation Center. Find a CBT pain therapist It can be hard to find psychologists trained in cognitive behavioral therapy for pain. Ask them about their approach to treatment. You might want to use the content from my pain truths and pain quiz to see if they match the latest pain science. Theres are links to therapist search tools and pain rehabilitation programs below. Learn more and do more
Image courtesy of McGovern Medical School
INSTEAD OF STARTING YOUR DAY WITH A LIMITED NUMBER OF SPOONS, YOU HAVE THE ABILITY TO SELF-CHARGE THROUGHOUT THE DAY TO BOOST ENERGY AND IMPROVE MOOD.
Christine Miserandino's spoon theory has become popular with people with chronic pain. It assumes people with chronic pain have only so much emotional and physical energy each day to do the things they want to do. You start each day with a finite number of spoons. Each spoon represents a unit of energy. As you use up your energy, you take away a spoon. While it's a helpful concept to help explain to friends and family who don’t experience chronic pain what it’s like to live with pain, the spoon theory is commonly used by chronic pain patients to plan their days so they don't over-extend themselves. The problem with the theory: there isn't a way to add more spoons (energy) or to make each spoon last longer than expected. Therefore, it can be self-limiting - focusing on what we can’t do instead of the things we can and leading us to avoid activities that could make us feel worse but may very well help us in terms of giving us more energy and improving our mood. For instance, we may choose to save spoons by not joining our friends for lunch or going on a much-needed walk. Recent research "demonstrated that on mornings when patients catastrophized more than usual about their pain in the day ahead, they spent more time in sedentary behavior and engaged in fewer minutes of moderate to vigorous physical activity that day. Cross-day lagged analyses further showed that the effect of morning pain catastrophizing on subsequent sedentary behavior extended to the next day. More time spent in sedentary behavior, in turn, contributed to greater pain catastrophizing the next morning" (Zhaoyang et al 2020). Who wants to wake up each day thinking you're limited in what you can do? I tend to see things more positively. We have more control over our pain, energy, and mood than we think. Another idea: Think of your day like a battery system in a car. If you don't use a car or if you leave on a car's lights or radio without the engine running, the car battery will eventually run out of energy. But if you drive the car, the alternator will recharge the battery as you drive. Just like a car's battery system, we can add more energy to our days by doing things like:
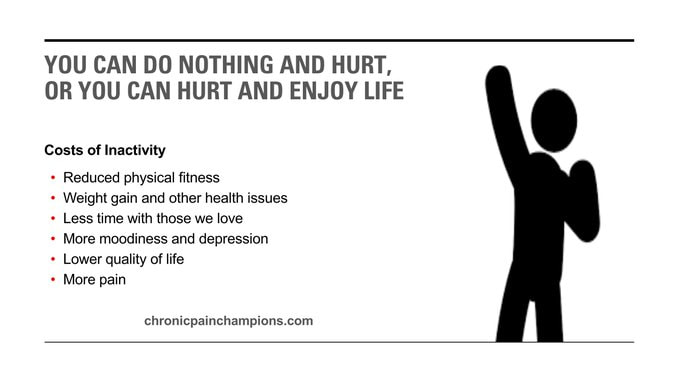
Check out 50 ways to live well, despite chronic pain. Note: This is just another tool to add to your chronic pain toolbox. If the spoon theory or another approach works for you, please continue using it. People with chronic pain often do too much when they’re having good days and not enough when they’re having bad days. Chronic pain can cause us to overprotect ourselves. Our natural reaction to pain is to avoid activities that worsen our discomfort or increase our perceived risk of further damage. When we become overly fearful and stop doing things in anticipation of pain, we can make things worse. Inactivity reduces our functional ability and decreases our strength and stamina. It also prevents us from getting involved in the social, leisure, and work activities we enjoy. Pacing/moderation has become a common tool for people living with chronic pain to help provide them with balance. It includes setting time limits, slowing down (start low, go slow), breaking up tasks, and taking frequent short breaks. But be careful not to let pacing become an excuse for not being active or avoiding pain. Doing so can add more focus to the pain, worsen symptoms, and reduce physical stamina. Pacing should instead be used to gradually increase what we can do, despite the pain. Stay consistent with your activity. The difference is in the goal and execution. Keep moving forward. Learn more and do more
Cooper, Booker and Spanswick, 2003
I just watched a great TEDx Talk from Dr. Trung Ngo about resilience that everyone who lives with chronic pain or treats chronic pain should watch.
He talks about how there are three types of people:
I can identify with all three types during my personal journey with pain. Early in my journey, I was the victim. It was the surgeon's fault for my pain. I was set on making that doctor pay for his mistake and make my pain go away. As the pain continued, I became the catastrophizer. It quickly became gloom and doom. I become fearful of the pain. I worried about all the terrible things that might happen because of the pain. And I worried about my future and the future of my family. Fortunately, my mindset changed to resiliency. Many thanks to the Mayo Clinic Pain Rehabilitation Center for helping me transition to that stage. How to be resilient According to Dr. Ngo, the keys to being resilient:
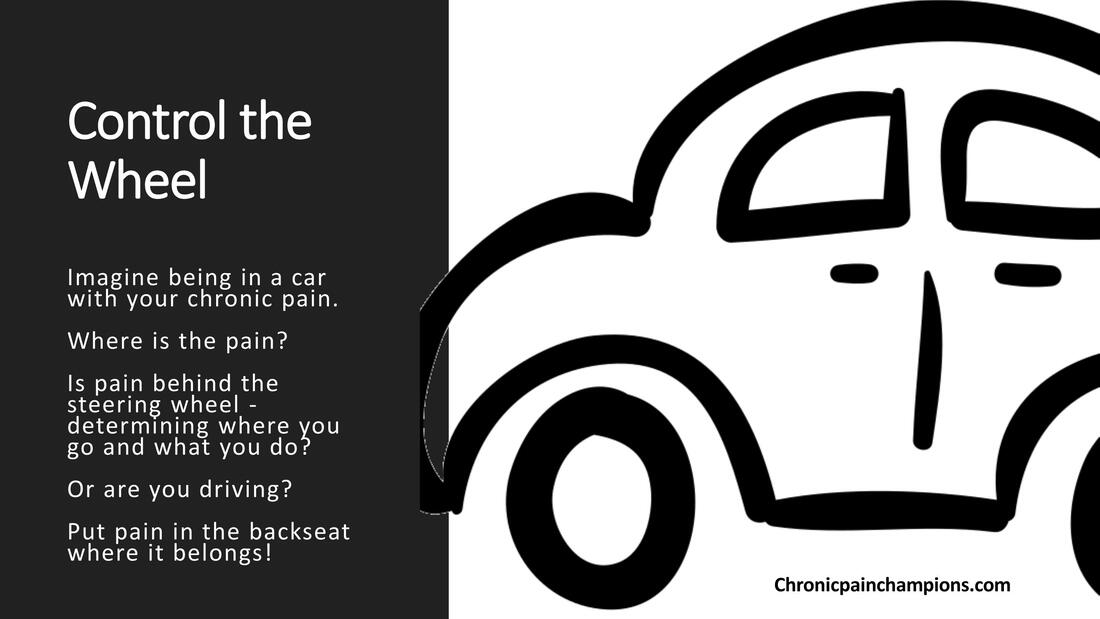
Learn more * Ojala, T., Häkkinen, A., Karppinen, J., Sipilä, K., Suutama, T., & Piirainen, A. (2014). Chronic pain affects the whole person – a phenomenological study. Disability and Rehabilitation, 37(4), 363–371. doi: 10.3109/09638288.2014.923522 I love this metaphor about who's driving the car - you or your pain.
Things you can control - Focus on these
Things you can’t control - Don’t focus on these
My article originally published December 30, 2019 in National Pain Report. Edited March 16, 2023 Chronic pain appointments can be difficult for both doctors and patients.
For patients, doctor visits can be intimidating and create anxiety. We want validation of our pain, empathy, answers, and support. For doctors, chronic pain patients can be more challenging to treat than other patients. We can be demanding of their time, attention, and patience. While they genuinely want to help, doctors often have limited training (typically only 11 hours of pain education in medical school); limited time (typically only 15-20 minutes per appointment); limited options due to government, health system, and insurance guidelines; and limited internal resources to treat chronic pain patients. So how do you make the most of your appointment time and get the best treatment when you visit the doctor? Below are 25 suggestions to help maximize the patient-doctor experience (thanks to the many ideas provided by members of the Chronic Pain Champions – No Whining Allowed Facebook support group): In general
Before the appointment
At the appointment
Bottom line To get the best treatment from your doctor, be prepared, calm, engaged, insightful, and open to self-management. It’s harder for doctors to treat patients who are negative or expect the doctor to fix all their problems. I hope you find these tips helpful. Chronic pain can make it easy to feel overwhelmed, reduce our activity levels, and become isolated. Goals help restore a sense of order, build self-efficacy and sense of control, improve mood, and provide direction by helping with planning daily activities.
One of the tools we learned at the Mayo Clinic Pain Rehabilitation Center was goal setting to help us plan our days and keep us on track. We set goals each day. They didn't have to be massive, but they had to be SMART - specific, measurable, achievable, relevant, and time-bound.
Some SMART goal examples:
Did you notice none of the goal examples included pain reduction? Our focus should be on reducing stress, improving our quality of life and increasing functional ability and activity, not pain reduction. Focusing on pain reduction is an easy trap to fall into - leading to frustration and depression. Just as the homepage of my website says - we can live well, despite the pain. Celebrate! While it's natural to celebrate big goals, be sure to celebrate milestones along the way, as well as smaller victories. These celebrations keep us motivated along the way and help instill confidence. Resource Pain is the body’s alarm system. It’s designed to protect us from danger just like a home security system or a smoke detector. It’s the body’s normal response to acute tissue damage or injury and heals in normally 3-6 months.
But what happens when pain doesn’t go away? Once pain persists beyond the normal healing time, it becomes chronic - losing its warning function and becomes its own disease/condition. It’s an abnormal response (with or without obvious pathology). Although all pain hurts, not all pain indicates damage. We know what to expect from our pain by the very nature of it being chronic or ongoing. It’s not like getting burnt, twisting an ankle, or getting stung by a bee that needs protection until the injury has heals. Of course, any unexpected new pain should be investigated. Learn more
Pain, stress, and tension are closely related. Muscles tighten and put pressure on nerves resulting in even more pain.
It’s possible to activate your body’s natural relaxation response to help reduce the tension using mind-body tools like:
Helpful videos
Free Apps FIND MORE TOOLS AND APPS Updated 3/1/24
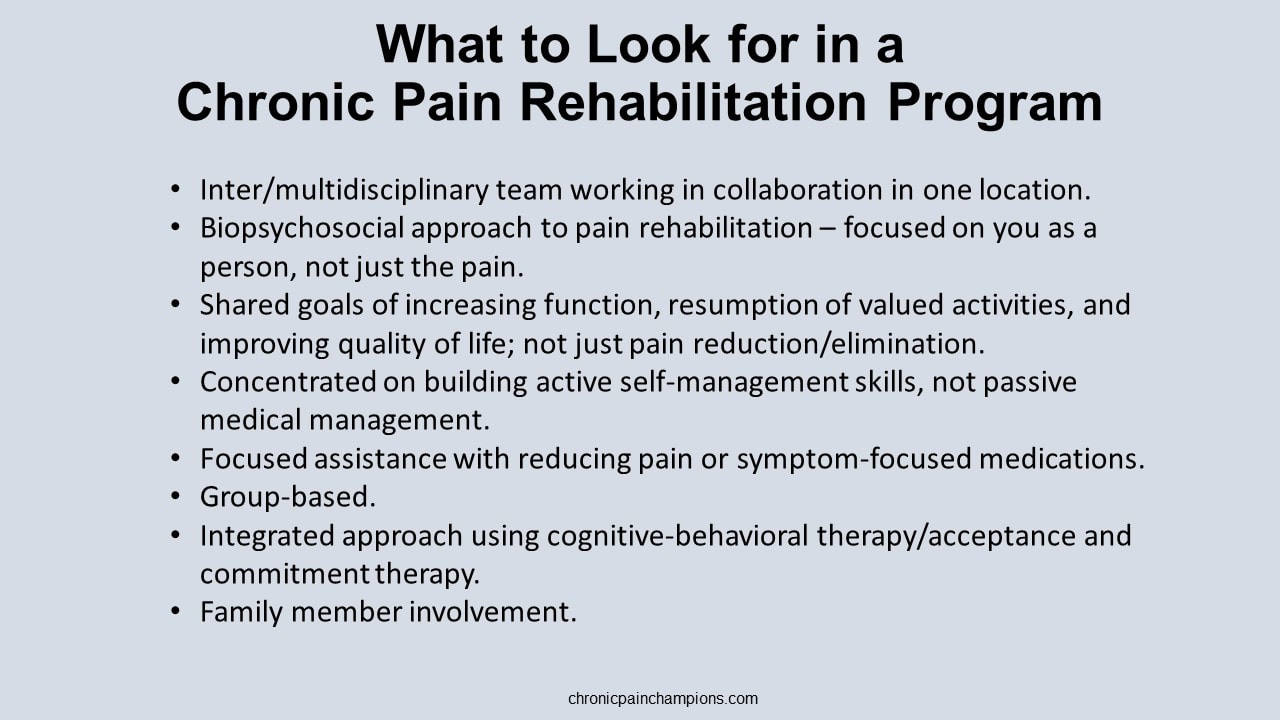
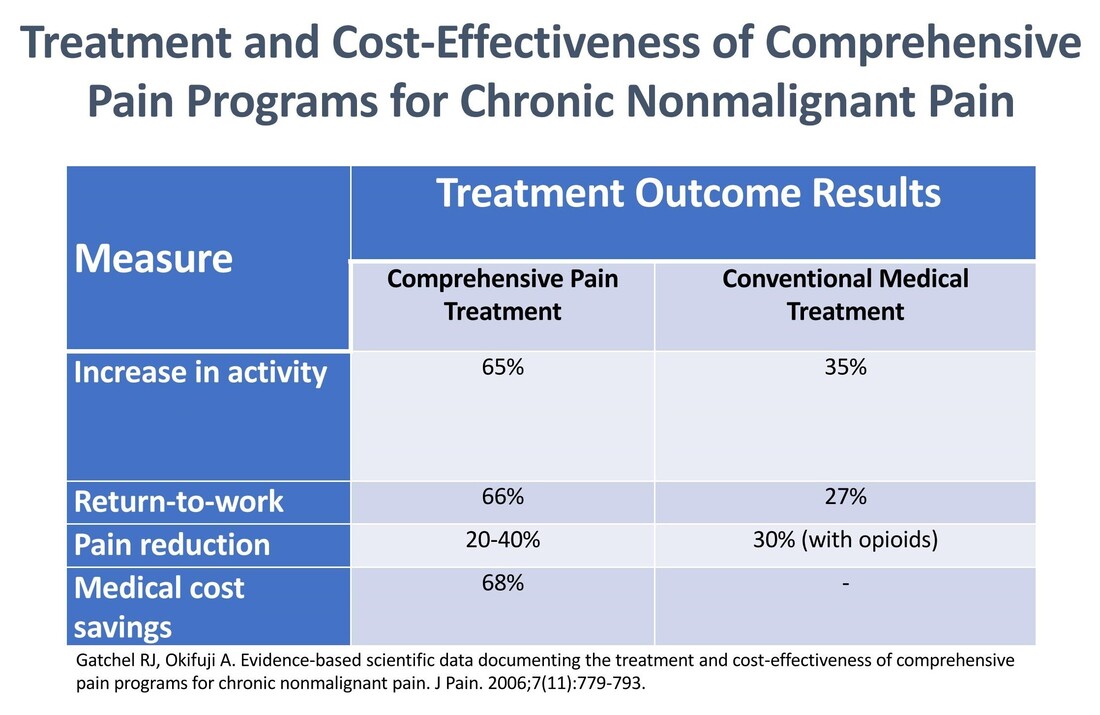
Pain rehabilitation goes beyond medicine and medical interventions – and crosses different disciplines. It doesn’t just focus on removing the pain. It focuses on the patient and how they can play a role in their own pain management - giving them control over the pain instead of letting the pain control them.. It’s a proven approach based on the biopsychosocial model of medicine – benefiting patients while reducing costs and reliance on the medical system. In addition to their general efficacy, these types of programs using interdisciplinary chronic pain rehabilitation can be effective at weaning patients off opioid therapy with long-term improvements in pain, mood, and function. I was fortunate to be able to attend the 3-week interdisciplinary Mayo Clinic Pain Rehabilitation Center – not just once, but twice. It was both a game-changer and lifesaver for me. I highly recommend the program to anyone interested in taking an active role in managing their own care. Read about my Mayo experience in this article. More programs like this are needed to shift the current reliance on biomedical therapy towards a greater reliance on provider-supported patient self-management and true biopsychosocial treatment. . Availability is important but so is accessibility. These programs aren't cheap, and insurance can be hesitant the pay the price tag. What payors need to remember is that these programs are cost-effective with a 68% reduction in medical cost spending. Find links to programs in the U.S. and around the globe. What to look for in a program A pain rehabilitation program should focus on you as a person, not just your pain. Interdisciplinary pain rehabilitation programs that take place in the same facility with health care providers working together with open communication and shared objectives are the gold standard of comprehensive care outperforming medical pain services and less coordinated multidisciplinary programs. A comprehensive pain rehabilitation program typically includes:
Learn more about pain rehabilitation
Pro golfers use visualization when they play. They picture the precise shot they want to hit before taking the club back – the trajectory, shape, roll and finish. This puts a positive image in the mind; the body then makes the motions needed to turn the image into reality.
We can do the same with our pain. We can visualize a different way to view our pain and respond to it. We can visualize living well despite the pain. And we can visualize the pain leaving our bodies or the pain taking a smaller role in our lives. Try these exercises
Find links to these and other self-management tools. I was recently honored to be a guest on the Compass Opioid Stewardship Program podcast hosted by Dr. Rachael Duncan, PharmD. and Dr. Don Stader.
I'm so grateful for the opportunity and blessed to be able to share my story with clinicians. I'm also thankful for the generosity of Dr. Stader. You'll find out what he offered me at the end of the podcast. It brought me to tears. You can listen to the podcast episode on Apple, Spotify, and Libsyn via the links below: Check out the entire podcast series. Learn more about the Compass Opioid Stewardship Program. |
Categories
All
Archives
July 2024
CHRONIC PAIN CHAMPIONS, LLC AND THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
All information is for educational purposes only. Use at your own risk. By accessing/using this website and any related pages/information/products/services, you agree to the terms and conditions. PLEASE SEE THE DISCLAIMER PAGE TO LEARN MORE. ©2024 Chronic Pain Champions, LLC All rights reserved. For personal, non-commercial use. |