|
(Updated 06/10/2024)
My article published in Health Central (formerly Practical Pain Management) "We Have a Chronic Pain Problem, Not a Prescription Opioid Problem" explored the efficacy and safety of opioids for chronic pain as well as the need for more pain rehabilitation programs. Below is some of the original content I submitted that didn't make the published version of the article which helps provide some additional context. The rise of prescription opioids In the 1990s and the next two decades, opioid prescriptions became the quickest and least expensive treatment option for chronic noncancer pain. Their rise in popularity was due to a mix of factors, including:
With the increase in opioid use came an increase in opioid use disorders and opioid deaths. Then came a hard push to reduce opioid prescriptions following the 2016 Centers for Disease Control (CDC) guidelines for prescribing opioids. The 2016 CDC guidelines indirectly led to many chronic pain patients being forced to lower their medicine doses or to stop them completely. Often with little or no tapering and no alternative treatments offered or covered by insurance. Pushing patients to undergo invasive procedures like injections or surgery. And labeling patients as “addicts” for wanting pain relief. Which all led to increased tension between patients and providers, more patient suffering, illegal drug use, or, even worse, suicide. Opioid users don’t know what they don’t know – “try it, you may like it” Unfortunately, there isn’t a crystal ball when it comes to pain treatment. There's no way of knowing how a patient will respond to any specific type of therapy. And tapering can be hard. Chronic pain patients can be weary of tapering opioids for fear of increased pain and the general fear of the unknown. Patients need to accept the possibility of worse pain and other symptoms during a taper. It’s also important for providers to remember to treat the entire person in pain and not just manage the taper. Transitioning to self-management built around pain rehabilitation takes time. It’s a marathon, not a sprint, and requires work from both the provider and the patient. It’s like the old joke “How do you get to Carnegie Hall? Practice, practice, practice.” Opioid treatment is a decision between the provider and patient The use of opioids is a shared provider-patient decision based on risk and reward including the history and needs of the patient and should be applied on a case-by-case basis. If the decision is to reduce or stop opioid therapy, tapering should be done with education about the benefits of opioid reduction and provider oversight. If the decision is to use opioids, they should be prescribed at the safest lowest dose. Either decision should include pain rehabilitation and self-management strategies.
Personal note My chronic pain recovery started after I accepted the pain and stopped doctor-shopping to find pain relief and a medical cure (many praises for the Mayo Pain Rehabilitation Center). Through pain rehabilitation, I learned how to self-manage my condition. This process led me to stop the use of medicines including opioids, benzodiazepines, anticonvulsants, muscle relaxers, amphetamines, beta-blockers, antidepressants, and over-the-counter analgesics as well as other passive interventions like supplements and injections for my pain.
There's still a core you despite the pain.
What you can do
Updated 7/19/24
Do you know?
Editor’s note: This article was written based on my experience and what I have researched about the topic. Everyone is different. The decision to use supplements should be a decision between the doctor and the patient. Many people use supplements are as part of their pain treatment approach, supplements come with risk, including contamination with toxins, health problems, unwanted side effects, and interactions with conventional medicines. Limited oversight Unlike prescription or over-the-counter drugs, which must be approved by the Federal Drug Agency (FDA) before they can be marketed, the FDA doesn’t review supplements for safety and effectiveness before they are sold. We don’t know where the products are made, how they are made, what is in them, and if the dosage is appropriate. Safety is left up to the manufacturers and distributors of the supplements. My experience As part of the multi-day Mayo Clinic fibromyalgia program I attended in 2016, I met with a pharmacist to review the long list of prescription medicines, over-the-counter medicines, and supplements I was taking at the time. My medicine cabinet looked like a GNC store. I was instructed to bring the actual bottles with me to the appointment, so I packed the bottles into a gym bag (yes, I was taking a lot of medicines and supplements) and went to see her. I was surprised as she read each bottle, making comments and recommendations about each pill – including product quality, labeling issues, ingredient safety, and dosing. When the appointment ended, my medicine and supplement list was much shorter with her recommending stopping most of the supplements and my gym bag much lighter – throwing away the pills was going to stop taking. I kept only one supplement - Vitamin D. Bottom line You assume all risk when using supplements. While some may be helpful, many aren’t and some may even be harmful. And remember, that each time you take a pill or supplement, you are reminding yourself you're in pain - reinforcing the neural pathways and keeping you in the pain cycle. Review any supplements with your medical team to help you make an educated decision. Learn more
Do you talk about the pain or complain about it? What do you do if other people ask you about the pain?
Pain talk is a maladaptive pain behavior – worsening symptoms by adding more attention to the pain. We can't move forward if we're constantly reminding ourselves of the pain or if we 're surrounded by negativity. I choose not to talk about the chronic pain i feel to myself or with others, including my doctors (unless there is a new symptom that need acute treatment). Learn more
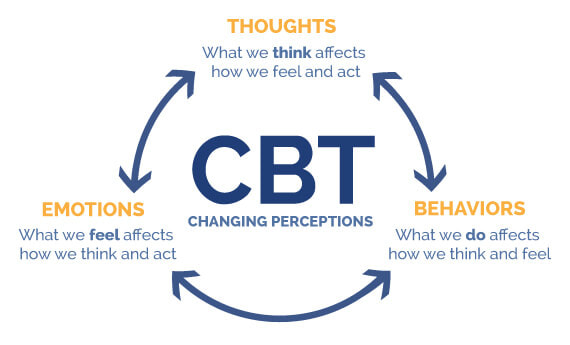
Updated 09/23/2023 Our thoughts, emotions, and behaviors can make pain worse or more manageable. We can change the pain experience and retrain our overprotective pain systems by changing how we think, feel, and behave using a form of biopsychosocial treatment called Cognitive Behavioral Therapy (CBT). CBT reprograms our minds and bodies to help us feel safe and confident in our ability to manage pain and do the things we enjoy — improving the body’s natural pain relief mechanisms, increasing function, and breaking the chronic pain cycle. .CBT is based on the core principles that our thoughts, emotions, and behaviors interact together with the pain; that we can become trapped in unhelpful thoughts, emotions, and behaviors; and that we can modify our thoughts, emotions, and behaviors to make our experience more manageable. It's what changed my pain experience and my life by giving me tools to:
Best yet, CBT is a do -it-yourself therapy. You can use it anytime. You don’t need help from anyone once you learn it. And there are no negative side effects. I learned CBT while attending the prestigious 3-week interdisciplinary Mayo Clinic Pain Rehabilitation Center. Find a CBT pain therapist It can be hard to find psychologists trained in cognitive behavioral therapy for pain. Ask them about their approach to treatment. You might want to use the content from my pain truths and pain quiz to see if they match the latest pain science. Theres are links to therapist search tools and pain rehabilitation programs below. Learn more and do more
Image courtesy of McGovern Medical School
|
Categories
All
Archives
July 2024
CHRONIC PAIN CHAMPIONS, LLC AND THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
All information is for educational purposes only. Use at your own risk. By accessing/using this website and any related pages/information/products/services, you agree to the terms and conditions. PLEASE SEE THE DISCLAIMER PAGE TO LEARN MORE. ©2024 Chronic Pain Champions, LLC All rights reserved. For personal, non-commercial use. |